Eye Conditions
Pacific Retina Specialists, Dr. David Parks specializes in the treatment of retinal diseases, including age-related macular degeneration. We also treat retinal detachments and the ocular complications of diabetes, ocular inflammatory diseases, and AIDS-related eye diseases. Other conditions we treat include:
- Age-related Macular Degeneration
- Diabetic Retinopathy
- Central Serous Chorioretinopathy
- Retinal Detachment
- Flashes and Floaters
- Macular Holes
To learn more about how we can treat retinal diseases, contact our practice serving Beverly Hills, Lancaster, and Guam.
Age-related Macular Degeneration (AMD)
As the population of California ages, we are experiencing an increase in age-related macular degeneration cases at our eye care centers. AMD is a common eye disease associated with aging that gradually destroys sharp, central vision. Central vision is needed for seeing objects clearly and for common daily tasks such as reading and driving. In some people, age-related macular degeneration advances so slowly that it will have little effect. But in others, the disease progresses faster and may lead to a loss of vision in one or both eyes.
How Does AMD Damage Vision?
The retina is a paper-thin tissue that lines the back of the eye and sends visual signals to the brain. In the middle of the retina is a tiny area called the macula. The macula is made up of millions of light-sensing cells that help to produce central vision.
AMD occurs in two forms:
- Dry AMD – Ninety percent of all people with AMD have this type. Scientists are still not sure what causes dry AMD. Studies suggest that an area of the retina becomes diseased, leading to the slow breakdown of the light-sensing cells in the macula and a gradual loss of central vision.
- Wet AMD – Although only 10 percent of all people with AMD have this type, it accounts for 90 percent of all blindness from the disease. As dry AMD worsens, new blood vessels may begin to grow and cause "wet" AMD. Because these new blood vessels tend to be very fragile, they will often leak blood and fluid under the macula. This causes rapid damage to the macula and can lead to a quick loss of central vision.
Who Is Most Likely to Develop AMD?
The greatest risk factor is age. Although AMD may occur during middle age, studies show that people over age 60 are clearly at greater risk than other age groups. For instance, a large study found that people in middle age have about a 2 percent risk of getting AMD, but this risk increased to nearly 30 percent in those over age 75.
Other Age-related Macular Degeneration risk factors include:
- Gender – Women tend to be at greater risk for AMD than men.
- Race – Whites are much more likely to lose vision from AMD than Latinos and Asians, and those of African descent rarely develop AMD.
- Smoking – Smoking may increase the risk of AMD.
- Hypertension – High blood pressure, especially when poorly controlled, may increase the risk of AMD.
- Family History – Those with immediate family members who have AMD are at a higher risk of developing the disease.
Symptoms
Neither dry nor wet AMD cause any pain. The most common early sign of dry AMD is blurred vision. As loss of function in macular cells progresses, people experience gradual loss of central vision. Oftentimes, this blurred vision will go away in brighter light. Eventually, there will be a small, but growing blind spot in the middle of the field of vision.
The classic early symptom of wet AMD is that straight lines appear crooked. This is similar to the effect of looking through a fun-house mirror. This is caused by leaking fluid or even bleeding from the damaged vessels, which lifts the macula and interferes with its function. There may also be a small blind spot in wet AMD cases, causing central vision loss.
If you believe you have symptoms of age-related macular degeneration, contact Dr. Parks’ office for an evaluation. Early diagnosis and treatment is crucial.
How Is AMD Detected?
You are at risk of developing AMD if you are over age 60 and have had recent changes in your central vision. To look for signs of the disease, Dr. Parks will use eye drops to
No treatment currently exists for dry AMD, but it has been suggested that taking certain vitamins and minerals, such as lutein, zeaxanthin and zinc, may slow the progress of the disease. A national study, called the Age Related Eye Disease Study (AREDS 2) published its results in 2013, exhibiting that a specific combination of vitamins and nutrients, including vitamin C, vitamin E, zinc, lutein, and zeaxanthin reduced the progression of dry AMD. At present, we recommend this combination, available commercially as Ocuvite Preservision AREDS 2, as well as other brands containing the AREDS 2 formula. We also recommend a balanced diet that includes many leafy green vegetables that are high in lutein. If you are unable to eat a balanced diet, a general multivitamin such as Centrum should be considered. There are many specialty vitamins touted to be good for macular degeneration, but because there is no conclusive evidence of their necessity, they are not recommended by Dr. Parks.
In September 2005, Dr. David Parks began offering Avastin (bevacizumab) for the treatment of neovascular age-related macular degeneration. Avastin (bevacizumab) works by blocking the effect of vascular endothelial growth factor (VEGF), one of the causes of abnormal blood vessel growth in age-related macular degeneration.
Avastin (bevacizumab) is available at all of our offices in the Los Angeles area and Guam.
Avastin (bevacizumb) is administered as an intraocular injection in the office under local anesthesia. Most patients experience no discomfort with the procedure. At present, retreatment by reinjection is recommended at four to six-week intervals for up to two years, depending on the response to treatment.
Avastin® (bevacizumab) is a medication that blocks blood vessel growth that is currently FDA approved for intravenous administration for colon cancer. Avastin® is not approved for ophthalmic use at this time. Recent studies have shown that Avastin® is be effective for macular degeneration and diabetic macular edema when injected in small amounts directly into the eye.
Avastin® (bevacizumab) is administered as an intraocular injection in the office under local anesthesia. Most patients experience no discomfort with the procedure. At present, retreatment by reinjection is recommended at four to six week intervals. The duration of treatment is depends on the individual response of the patient, with some needing treatments for a few months and others many years.
Avastin® (bevacizumab) is available at all of our offices in the Los Angeles area and Guam.
Lucentis™ (ranibizumab) is an anti-VEGF drug manufactured by Genentech. In July, 2005, Genentech released the results of a study demonstrating that 95 per cent of patients with macular degeneration treated with Lucentis™ lost fewer than 15 letters of vision compared to 62 percent of untreated patients. More importantly, nearly one third of Lucentis™-treated patients showed an improvement in vision compared to only 5 percent of untreated eyes. In November, 2005, Genentech released results of another study that compared Lucentis™ to Visudyne™ without supplemental intraocular triamcinolone. This study demonstrated that 94 to 96 percent of Lucentis™-treated patients maintained or improved vision. Lucentis™ was FDA approved in 2006 and has been available in all of our offices since that time. Genentech, Inc. is the manufacturer of both Avastin® and Lucentis™. Genentech is not involved in any the trials evaluating Avastin® for treatment of wet AMD. This is an off-label use that the company has so far declined to support.
Eylea (aflibercept) is another anti-VEGF drug that is manufactured by Regeneron and was FDA approved in 2011. It has a minor advantage over Avastin and Lucentis in a longer duration of action, lasting up to eight weeks in some patients. Because of this, some patients who need ongoing or indefinite therapy require less Eylea injections per year, compared to Avastin and Lucentis.
In addition to injections, Dr. Parks can treat some cases of wet age-related macular degeneration at both our Los Angeles and Guam offices with two types of laser surgery. Thermal laser surgery has been proven to be effective in the treatment of wet AMD lesion for almost 15 years. This treatment involves aiming a strong light beam onto the new blood vessels, essentially destroying them. All patients may go home the same day, but must return for a follow-up exam and angiogram within the next month. A second type of laser treatment, known as ocular photodynamic therapy, has been FDA approved and available in Dr. Parks' office since April 2000. In involves the intravenous infusion of a green photosensitive dye, called Visudyne (verteporfin). This is immediately followed by a one-and-a-half-minute treatment with a low-intensity infrared laser, which is not much different from the red laser emitted by a laser pointer.
For more information regarding the many treatments for macular degeneration, contact the office of David Parks, a Southern California retinal specialist. Also, you may visit the Web sites maintained by the manufacturers of the approved:
- Avastin® (bevacizumab)
- Lucentis™ (ranibizumab)
- Eylea (aflibercept)
- Visudyne™ (verteporfin)
- Macugen® (pegaptanib)
Our office recognizes that some of these medications, especially Lucentis (ranibizumab) and Eylea (aflibercept), are expensive. Our staff is adept at exploring all options, such as copay assistance programs or free drug programs for those in need who cannot afford these sight-saving drugs or their insurance copayments.
Diabetic Retinopathy
Diabetes can cause all sorts of health problems, including diabetic retinopathy. Diabetic retinopathy is a disease in which the retina is starved of oxygen and ultimately damaged. The condition develops when a patient's blood sugar levels surge, causing severe injury to the blood vessels that supply oxygen to the retina. The vessels often begin to function poorly and can even leak fluid into the center of the retina, called the macula. This fluid accumulation, called nonproliferative diabetic retinopathy, can cause mild to severe vision loss. Other complications include macular swelling, called macular edema, which can also lead to impaired vision. When treated properly, diabetic retinopathy and its effects are reversible; when ignored, it can lead to permanent vision loss and other health problems.
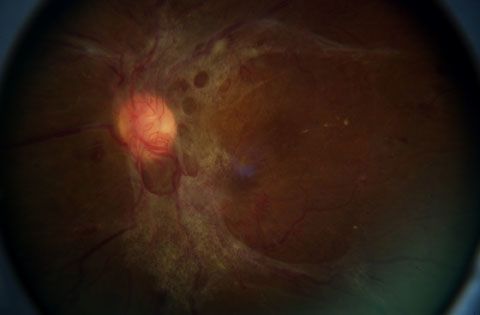
Diabetic retinopathy is a condition that affects the retina.
Who Is Most at Risk for Diabetic Retinopathy?
Anyone with Type I (juvenile onset) or Type II (adult onset) diabetes is at risk. Additionally, diabetic pregnant women are particularly susceptible to diabetic retinopathy. We recommend that all diabetic pregnant women have dilated eye examinations each trimester to protect their vision.
What are the Symptoms?
Diabetic retinopathy often has no early warning signs. At some point, though, you may develop macular edema, which blurs vision, making it hard to do things like read and drive. In some cases, your vision will get better or worse during the day. As new blood vessels form at the back of the eye, they can bleed (hemorrhage) and blur vision. The first time this happens it may not be very severe. In most cases, it will leave just a few specks of blood, or spots, floating in your vision. They often go away after a few hours. These spots are often followed within a few days or weeks by a much greater leakage of blood. The blood, too, will blur your vision. In an extreme case, one will only be able to tell light from dark in that eye. It may take the blood anywhere from a few days to months or even years to clear from the inside of the eye. In some cases, the blood will not clear. Also, you should be aware that large hemorrhages tend to happen more than once, often during sleep.
Importance of Treating Diabetes
How Is It Detected?
Diabetic retinopathy is detected during an eye examination that includes:
- Visual acuity test: This eye chart test measures how well you see at various distances.
- Pupil dilation: The eye care professional places drops into the eye to widen the pupil. This allows him or her to see more of the retina and look for signs of diabetic retinopathy. After the examination, close-up vision may remain blurred for several hours.
- Ophthalmoscopy: This is an examination of the retina in which Dr. Parks examines the eye either by looking through a device with a special magnifying lens or, wearing a headset, uses a bright light to look through a special magnifying glass to get a good look at the retina.
- Tonometry: A standard test that determines the fluid pressure inside the eye. Elevated pressure is a possible sign of glaucoma, another common eye problem in people with diabetes.
We will use these tests to screen for early signs of the disease, such as:
- Leaking blood vessels
- Retinal swelling, such as macular edema
- Pale, fatty deposits on the retina – signs of leaking blood vessels
- Damaged nerve tissue
- Any changes in the blood vessels
Many times we also do a more thorough test, called fluorescein angiography, during which a special dye is injected into the arm and photographed as it passes through the blood vessels in the retina. This test allows us to find leaking blood vessels and to target them during laser surgery.
How is Diabetic Retinopathy Treated?
There are several treatments for diabetic retinopathy: laser surgery, intraocular injections of medications to reduce retinal swelling or to suppress blood vessel growth, and vitrectomy. Combinations of these treatments are very effective in reducing vision loss from this disease. In fact, even people with advanced retinopathy have a 90 percent chance of keeping their vision when they are treated early. However, it is important to note that although these treatments are very successful, they do not cure diabetic retinopathy, and they also do not cure your underlying diabetes.
What Can You Do to Protect Your Vision?
Pacific Retina Specialists urges everyone with diabetes to have an annual dilated-pupil eye examination. For those who have developed serious retinopathy, Dr. Parks will suggest a schedule of more frequent examinations.
According to a recent study by the Diabetes Control and Complications Trial (DCCT), effective control of blood sugar levels slows the onset and progression of retinopathy, as well as reducing the need for laser surgery for severe retinopathy. Study participants who kept their blood sugar levels as close to normal as possible had much less eye, kidney, and nerve disease. Elderly patients, children under 13, and patients with heart disease should consult a doctor for guidance in blood sugar control for retinopathy, since there are other considerations applicable to them.
For more information about diabetic retinopathy or diabetes, you may wish to contact:
Central Serous Chorioretinopathy
Central serous chorioretinopathy, the collection of fluid under the retina, results in visual distortion. As the name suggests, this condition most seriously affects central vision.
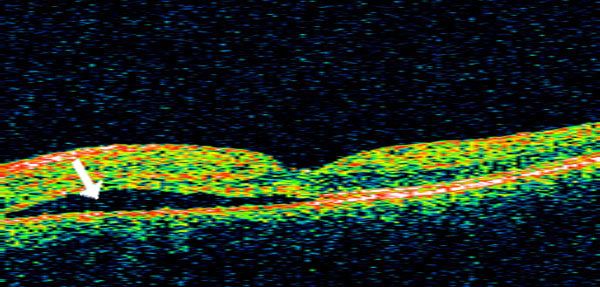
Central serous choroidoretinopathy can cause visual distortion.
Symptoms
Patients often complain of a blind spot, decreased or blurry vision, and distortion of shapes such that straight lines may appear bent or crooked. The vision may be minimally to significantly affected, with visual acuities ranging from normal (20/20) to 20/200.
Who Is at Risk?
The disease primarily affects young adults ages 20 to 45. Men are affected ten times more frequently than women. Coincidentally, many patients tend to live very stressful lives.
What Causes Central Serous Choroidoretinopathy?
The exact cause of central serous choroiretinopathy is highly controversial. However, there appears to be an imbalance in the amount of fluid that enters the subretinal space and the ability to remove it, resulting in a net accumulation of fluid beneath the retina. Some experimental evidence suggests high blood levels of epinephrine and cortisol hormones may be responsible.
Prognosis
Most patients with central serous chorioretinopathy will spontaneously recover visual acuity in six months (average time to recovery three to four months). Many patients will have some residual symptoms, such as distortion, decreased color and contrast sensitivity, and visual difficulty at night. Despite an overall good prognosis, 40 to 50 percent of patients experience at least one recurrence.
Is There Any Treatment Available?
There is no medical therapy proven to be effective in treating central serous chorioretinopathy.
We do treat patients with two types of laser.
Photodynamic therapy, (PDT) involves the intravenous injection of a green dye, called Visudyne (verteporfin) over a ten minute period. After five minutes, a “cold” laser treatment is applied to the affected area of the retina, previously determined by a diagnostic test called fluorescein angiography. The dye will leak or concentrate in the diseased part of the retina and the laser can then target the dye, closing the leaks in the tissue under the retina.
Thermal laser photocoagulation treatment is also used when the affected area of the retina is not in the center of the macula. It is said to shorten the duration of the disease; however, it does not appear to alter the final visual acuity or the recurrence rate.
Retinal Detachment
Retinal detachment occurs when the retina lifts and detaches from the rear wall of the eye, causing total, and if not properly treated, permanent vision loss. The surgeon is usually initially most concerned with whether the macula – the retina’s center – is still intact. This is crucial because the macula controls central vision. In addition, the resulting state of the macula determines what type of surgery is needed.
Symptoms
Symptoms include a sudden or gradual increase in the number of floaters and/or light flashes in the eye or the appearance of a curtain over the field of vision. A retinal detachment is a medical emergency. Anyone experiencing the symptoms of a retinal detachment should call our office or arrange to see an eye care professional immediately.
Types
There are three different types of retinal detachment, including:
- Rhegmatogenous [reg-ma-TAH-jenous] – With this type, a tear or break in the retina causes it to separate from the retinal pigment epithelium (RPE), the pigmented cell layer that nourishes the retina, and fill with fluid.
- These types of retinal detachments are the most common.
- Tractional – In this type of detachment, scar tissue on the retina's surface contracts and causes it to separate from the RPE. This type of detachment is less common.
- Exudative – This type is frequently caused by retinal diseases, including inflammatory disorders, and injury/trauma to the eye. It is marked by the leaking of fluid into the area underneath the retina (subretina).
Who Is at Risk for Retinal Detachment?
Although anyone can experience a retinal detachment, people with certain eye conditions are at increased risk. People who are very nearsighted can have thinning and weak spots in parts of the retina that make them susceptible to developing a retinal tear or detachment. Other risk factors for retinal detachment include posterior vitreous detachment, lattice degeneration, x-linked retinoschisis, degenerative myopia, and uveitis. Injuries to the eye or head can also cause retinal detachment.
How Is Retinal Detachment Treated?
Small holes and tears are treated with laser surgery or a freeze treatment called cryopexy. Both of these procedures are available in Dr. Parks' office. During laser surgery, tiny burns are made around the hole to weld the retina back into place. Cryopexy is a similar procedure that freezes the area around the hole.
Larger retinal detachments are treated with surgery that may require the patient to stay in the hospital. In some cases, a scleral buckle, a tiny plastic band, is attached to the outside of the eyeball to gently push the wall of the eye against the detached retina. If necessary, a vitrectomy may also be performed to treat more severe cases. During a vitrectomy, Dr. Parks makes three tiny incisions in the sclera (white of the eye). Next, a small instrument is placed into the eye to remove the vitreous. Salt solution is then injected to into the eye through an incision to replace the vitreous. The third incision is for a fiber optic light pipe to allow the surgeon to see inside the eye during the surgery. As always, early treatment can usually improve the vision of most patients with retinal detachment, but some patients will need more than one procedure to repair the retina.
Flashes and Floaters
Flashes of light are caused by the tugging of the vitreous in the spot where it is attached to the retina. As the vitreous gel pulls on the retina, the brain interprets this as flashes of light. Conversely, once the vitreous gel has liquefied and separated from the retina's surface, the vitreous gel may condense and the patient may see fine strands and strings in his or her vision. Since these seem to float, they are called floaters.
Flashes and floaters are usually associated with a combination of aging and/or nearsightedness. Most of the time, they are a normal consequence of aging and become less noticeable with time. However, patients should be examined at the onset of these symptoms to make sure no other more serious conditions (such as a retinal tear or detachment or posterior vitreous detachment) are present.
Treatment of symptomatic floaters
The treatment of floaters is controversial. Historically, retinal eye surgery was a risky treatment and most retinal surgeons did not recommend any treatment for floaters since it was not felt to be a sight threatening disease.
Around 2000, new advances in retinal surgery were made, including reduction of incision size from 20 gauge (the size of a needle used for taking a blood test) to 23, 25, and now 27 gauge. This results in an incision that is less than half the size, and does not need stitches to close.
Dr. Parks now offers 27 and 25 gauge small incision, sutureless vitrectomy surgery for the treatment of symptomatic floaters. As this treatment is still not widely accepted by all retina surgeons, our office is compiling our surgery data in a research study to determine the safety and efficacy of this procedure. Presently, people with symptomatic floaters who are over age 50 and have had severe symptoms for more than six months are screened as possible candidates for this procedure.
Laser surgery is also offered by some ophthalmologists for the treatment of symptomatic floaters. At present, Dr. Parks does not believe this is a safe or effective procedure and does not perform this procedure.
Macular Holes
The round shape of the eye is maintained by vitreous, a substance with the consistency of soft gelatin that fills the central eye. With age, the gel shrinks and shifts toward the front of the eye, pulling away from the surface of the retina. The body replaces the lost gel volume with natural fluid. For most people, the process presents no serious consequences beyond developing a few floaters. For a few, however, the attachment of the vitreous to the retina may be strong enough that the pull of the contracting vitreous can create a hole in the central retina, known as a macular hole. The replacement fluid may seep through the hole, lifting the retina and causing distortion in central vision.
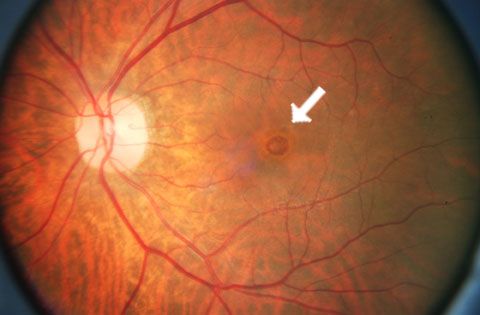
A macular hole can develop as a result of pressure from the vitreous.
Symptoms
A macular hole causes decreased central focus for both near and distance vision, and a loss of vision in a small central area. To confirm a macular hole, Dr. Parks will perform a detailed retinal examination. This may include a fluorescein angiogram, in which photographs are taken of the back of the eye after a special dye has been injected into the blood.
Treatment
To treat a macular hole, Dr. Parks will perform a vitrectomy. The first step is to remove the vitreous from the eye, to ensure there is no further pulling of the retina.
Next, a large gas bubble is placed into the eye, to exert gentle pressure to return the retina to its original position, forcing the fluid back through the hole and securing the retina to the rear surface of the eye. To work most effectively, the gas bubble must be pushing up, which means the patient must spend a week or two in a face-down position. Dr. Parks can recommend some devices available from medical equipment rental dealers to help maintain the face-down position while eating, reading, and sleeping.
After about six to eight weeks, the gas bubble will be absorbed by the body and replaced with natural saline fluid. The patient can then be measured for glasses.
A vitrectomy is normally performed under local anesthesia. Some patients may require an overnight hospital stay. An examination is performed shortly after the procedure, as well as regular follow-up examinations for about three weeks, to monitor the closure of the hole and watch for complications and reinforce the need to remain face down. Eye drops will be prescribed to alleviate irritation and reduce the chance of infection.
A vitrectomy will often cause cataracts in the patient within six months to two years. This will require lens replacement surgery.
A small percentage of vitrectomy patients will suffer retinal tears or detachments, which can be corrected with further surgery.
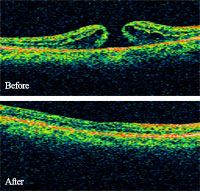
Macular Holes - Before and After
Macular Holes and Macular Degeneration
Macular holes and macular degeneration are not related. A macular hole is caused by the vitreous pulling on the front of the retina, while macular degeneration is caused by changes to tissue behind the retina.
Are Macular Holes an Inherited Trait?
There is no evidence to date to suggest that the likelihood of developing macular holes is related to genetic inheritance.
Does a Macular Hole in One Eye Predict a Hole in the Other?
While there is no certainty that both eyes will suffer the same problems, Dr. Parks will examine the untreated eye to evaluate the vitreous gel and the extent of its traction on the retina. If complete separation has occurred, there is little chance of a macular hole. If, however, there is significant traction, the other eye should be carefully monitored.